It was a Monday-- the start of a fresh semester. I pushed through a weird queasy/cramping feeling in my stomach all day and happily attended night class. Following class, I went to bed feeling completely nauseated and incredibly exhausted from "pushing through" all day. Still, it didn't occur to me that something could be seriously wrong.
Around 2am Tuesday morning I began throwing up. I woke up sweating profusely with a fever of 101.2 and attempted to go back to sleep + ignore the pain in my stomach though it appeared to be worsening. At this point, I thought perhaps I had the flu. I had also done my Methotrexate injection the evening prior and it is not uncommon for me to experience nausea/vomiting/a low grade fever following injection night(s). I continued trying to get some rest. No big deal, I thought.
I was wrong.
By 8am Tuesday morning, I could no longer hold down water or lie in anything other than the fetal position. The "twisted" feeling in my stomach left me feeling pretty certain that I was suffering from a bowel obstruction. I picked up my phone and dialed the colorectal surgery office and spoke with one of the nurses who cared for me following my
subtotal colectomy last April. Through tears, I explained my symptoms and attempted to breathe deeply through the pain which was becoming more and more difficult to do as the seconds passed. The nurse and I both agreed that I needed to get to the Emergency Room where my attending surgeon would come by later. That said, she started the admitting process over the phone.
As I was giving the nurse the basic admitting information she asked for, she told me to pack a few things and gather my medications. Though I was aware of my delusional state from lack of sleep and the exhaustion that accompanies such pain, I somehow thought that I was going to drive myself to the ER. As I crawled my way out of bed and stood up to gather my medications, the pain became so severe that I blacked out/fainted. It happened quickly and absolutely without warning. When I came back "to" I was lying in a puddle of vomit and completely disoriented. After a few seconds, I remembered I had been talking to a nurse. I picked my phone off the floor and heard her say "McKenzie, stay with me. There is an ambulance on the way."
I don't know if it was the sheer feeling of defeat or the effects that the significant pain/lack of sleep were having on me at this point, but I broke down into hysterical sobs on the floor of my bedroom. Within 5 minutes, several paramedics came into my dorm room apartment, somehow managed to get me on the stretcher, and on the way to the hospital.
The ambulance ride was absolutely terrifying and incredibly uncomfortable. The pain continued to ebb and flow much more severely. As it lessened and then spiked again I screamed, continued to sweat, and white knuckled the scratchy ambulance blanket all wadded up in my hand. I really don't think I can even recount further details right now as my mind seems to be blocking them out (and for good reason). The 12 hours between 8am and 8pm that day were easily the worst and most painful hours in my 21 years of life thus far.
By the time we arrived at the hospital, all of my admitting paperwork was done. I was brought to a room in the ER where I was given pain meds and we arranged for a CT scan. The CT revealed (as suspected) a small bowel obstruction. Due to its location and severity, my surgeon suggested I may have had this obstruction for over a month.
Immediately, an NG tube was placed to decompress my stomach and remove the bile which had settled and was making me so sick. My surgeon came in again shortly thereafter and explained the emergency dilation procedure I would need to undergo early the following morning. At this point, my pain was being phenomenally managed and the next thing I remember is waking up in the hospital room I would call home for the next 7 days.
The days were long and the nights were even longer. Though my pain management regimen was very helpful in "taking the edge off," it was very evident that beyond the mechanical obstruction problem, we were dealing with significant inflammation all along my digestive tract. This inflammation can only really be treated by entire removal of the affected part(s) or utilizing high dosages of immunosuppressant drugs. Thus, the pain and symptoms continued as we began having conversations about permanent ileostomy/colostomy placement.
Around the 4th or 5th day, I remember lying in bed around 4pm. I had just turned on the song "In Control" by Hillsong United, closed my eyes, and quite literally began to cuss at God. Mere seconds after this argument began, in walked the hospital Chaplain. As we began talking he said "McKenzie, I remember you." It turns out this Chaplain had also come to visit with me back in April '16 when I underwent my subtotal colectomy. He remembered me as the youngest patient on that particular floor, and he also remembered a joke I had cracked in the midst of the hysterical tears that often accompany such post-op pain. Ha!
The Chaplain sat next to my hospital bed in an uncomfortable folding chair for a good hour. We talked about the complexity of my illnesses, how passionate I am about studying to become a social worker, and how I managed to get a hospital room "with a view." (Seriously! It had the best view of the Minneapolis skyline!) As we wrapped up our conversation, he asked to pray with me. Without thinking or really even knowing what was coming out of my mouth, I replied by saying "we can pray, but I don't want you to pray for me to be healed."
A bit taken aback but seemingly intrigued, the Chaplain looked and me and said "tell me more about that." Through tears and a continued whisper tone of voice (thanks, NG tube) I told the Chaplain things I have never told another human before. I told him what I feel God has been telling, showing, and teaching me for the past 7+ years.
I told the Chaplain I couldn't remember the last time I prayed true, physical healing over my own body. I told the Chaplain how I haven't
really been to church in over a year. I told him of some recent experiences in which two church "leaders" suggested there may be "unforgiven, generational sin" in my family...hence the reason I had not yet "received healing."
Finally, I told the Chaplain what I felt God was telling me as I had been lying in the that hospital bed. I told him that I had spent the past several days doing nothing but swearing and yelling at God. Angry...livid, really. But also that I had never felt so close the One who created my body this way...and no doubt for some good and holy reason.
I told the Chaplain that I believe God can heal. In fact, I believe that He
DOES. But there is something to be said about other forms of healing
(in ways and for reasons higher than our own) apart from the physical. I believe that God has been faithful to me thus far and will continue to be. I see that
God has used this pain whether He ordained it or not. He has made it purposeful, intricate, and beautiful. He has made it worthwhile. And yes, He has even made it
good.
"God could have healed me 7 years ago, a week ago, even yesterday...
but He has not chosen to do so...and
that," I shared, "gives me reason to believe that perhaps the path I'm walking has a purpose far greater than what I will ever be able to comprehend."
That, to me, is the absolute truth. Some way, some how, God has given me distinct purpose and great joy in a life marked by tragic illness, great despair, and exhausting desperation. Perhaps having been given those things is what allows me to live a better life than the one I would be living if physical healing allowed me to do so painlessly and "ailment free" here on earth.
The bottom line I tried to explain is that
to live in a constant state of pain is to live in a constant state of reliance on faith in Christ. I believe that and know nothing will ever compare to that. I fully believe that being healed and whole in Heaven one day will be worth the journey I am currently on.
Heaven. My mind was then directed to the idea of
Heaven. Through tears I told the Chaplain "I don't want to be healed because I want to experience the fullness of God's presence
HERE. In great sickness. In horrendous pain. In a plastic hospital bed with an NG tube down my throat, a defeated spirit inside of me, and visible tears in my eyes..."
I want to experience the fullness of Christ and how He responds to His children when they are lying awake at 2am screaming in pain and begging for the strength to make it through to the next dosage of pain meds. I want to experience the fullness of Christ which feels so visceral and overwhelmingly beautiful upon waking up from yet another round of general anesthesia. I want to experience the fullness of Christ in the deepest, darkest hours of my life here on earth.
...And I want those things not for attention, pity, or to be seen as some great martyr. I want those things and the other pain our broken lives bring because I want to seek, to know; to pursue, to learn. To wrestle with and experience the perplexing truth that authentic JOY is possible in the midst of severe pain.
All of these thoughts and tears had me reciting a favorite poem in my head. A poem that I'd never truly understood before, but could now grasp to its full extent.
The Thorn by Martha Snell Nicholson
I stood a mendicant of God before His royal throne
And begged Him for one priceless gift, which I could call my own.
I took the gift from out His hand, but as I would depart
I cried, "but Lord this is a thorn and it has pierced my heart.
This is a strange, a hurtful gift, which Thou hast given me."
He said, "my child, I give good gifts and I gave My best to thee."
I took it home and though at first the cruel thorn hurt sore,
As long years passed I learned at last to love it more and more.
I learned He never gives a thorn without His added grace,
He takes the thorn to pin aside the veil which hides His face.
I don't want to be (physically) healed. Not here, not now...for I
know God is using this daunting hike through life and the mountains of chronic illness to refine and restore my soul in ways that only He can.
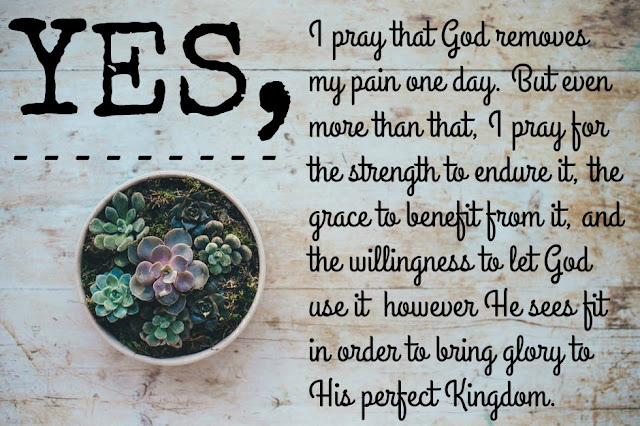
So, the Chaplain and I prayed. Not for physical healing but for the strength to endure. The grace to benefit. The willingness to learn from and let God
use this pain. For the first time in a long time, I felt like someone had truly listened to me. Someone allowed me to be comfortable in all of my uncomfortableness...someone chose to enter into that uncomfortableness
with me. And in my mind, there is nothing more beautiful than that.